Community roots, community reach
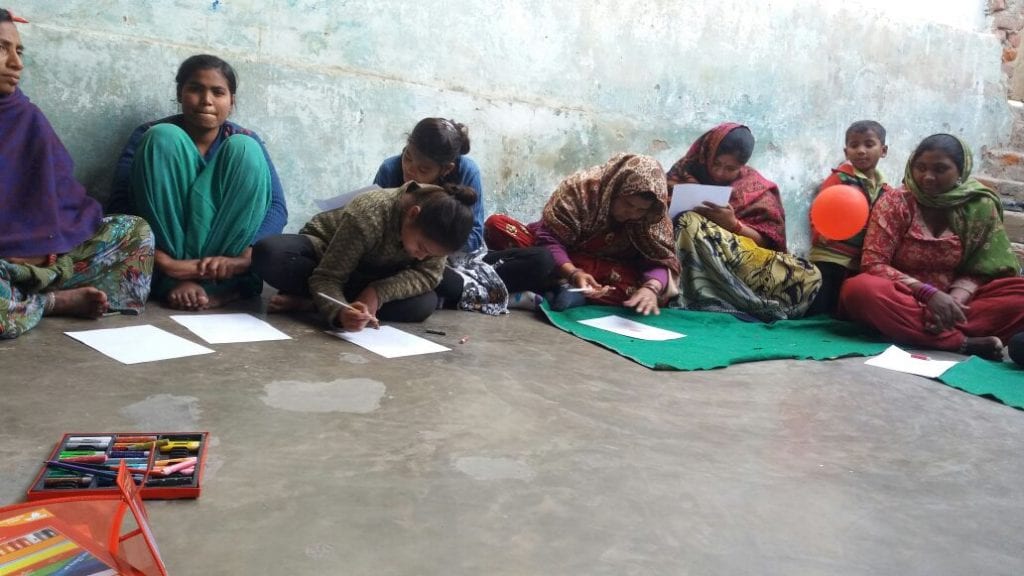
Chanda (name changed), along with eight other peer educators with a similar background, regularly visits families in an urban slum of New Delhi to talk with them about diabetes, hypertension, cancer and alcohol and tobacco. These peer educators are 15- to 18-year old students and are living in the same community where they conduct their interventions. That makes it easier for them to understand and to make a connection with the families they meet. Five out of nine peer educators share how their fathers were addicted to alcohol and despite being girls how they managed to make their fathers understand and help them overcome addiction. Building on their own stories and being able to rely on their intimate understanding of the community, the peer educators, like Chanda, are able to relate once they get a chance to speak with families that are affected by health issues. The peer educators are part of a program conducted by NADA India.
In the program, NADA peer educators learn how to develop connections that empower people in the community who are affected by alcohol and stress and are facing stigma. People suffering from alcohol problems or other diseases are usually blamed for their health issue by the close family, and are often trying to hide their problems from society due to stigma – which results in delay in treatment.
Preventing mental ill health, addressing stigma
The NADA Peer education program aims to meet the need in the community to engage patients before they accept this new identity of “patient” and promote informed choices among people effected and affected by NCD risk factors (tobacco use, unhealthy diet, insufficient physical activity and the harmful use of alcohol).
Evidence shows that brief psychological treatments for alcohol problems, based on motivational enhancement, are acceptable, feasible, and cost-effective, even when delivered by non-specialist health workers like peer educators and lay counselors in routine health-care settings in previously untreated populations. Such treatments should be scaled up as one of the resource.
Recently, I conducted a workshop for post graduate students from different colleges of Delhi in life skills. Many students approached me after the session, and they talked about their sufferings because of social isolation and anxiety. The biggest problem for them was to talk to someone about what is going on in their mind and they were afraid of being labelled as insane.

Today we can see around us how stereotypes about people with mental health problems, including alcohol dependence, are portrayed in movies, mass media and the press, with the use of derogatory terms such as “psycho” or “nut” or in Hindi “Paagal”. We see depictions of them as being violent and dangerous persons. This portrayal of mental ill health in popular culture becomes a major source of stress for people effected and affected by mental illness and addictions.
I think it is important to see stigma as a social process. Approaching stigma as a social process will allow us to understand how a stigmatized person at primary level is at risk of being ill not because of an inherent, unchangeable and irremediable attributes, but because of a social condition that puts him/her at risk.
Mental ill health is a massive burden
The total number of people living with depression in the world is 322 million. Nearly half of these people live in the South-East Asia and Western Pacific Region. According to WHO figures, the total cases of depressive disorders in 2015 in India were 56,675,969 which was 4.5% of the population. The WHO figures also show that total cases of anxiety disorders were 38,425,093 which was 3% of the population in the same year.
Mental ill health is a massive public health and developmental problem. In India, for instance, suicide is the leading cause of death in people aged 15 to 29 years.
Mental ill health is a widespread problem in my country, including depression and alcohol use disorders. Alcohol problems drain the household budgets, especially concerning already marginalized and vulnerable people. It can significantly strain family budgets, due costs for NCD-related health care and medicines. Costs for alcohol diverts the household’s income and resources from ensuring food and nutrition security and from basic education. Furthermore, alcohol harm also strains the public budget, due to healthcare, law enforcement, economic and social costs. In addition, the treatment gaps are still huge.
Communities – catalysts for change
In a situation like this, what we are missing is empowered communities where people are connected and enabled rather than isolated because of a (mental) health condition.
It can be seen that increasing the budget outlay is not enough if states do not have the human resources or the infrastructure to respond to social determinants of health. One allopathic doctor in a government hospital serves an average population of 11,528 people, according to data from the National Health Profile 2015.

Substantially, research indicates that supportive social networks of friends, relatives and other social contexts mitigate the damaging painful life stresses. In contrast people deficient of social networks may respond to negative life stress by becoming severely depressed resorting to alcohol or other drugs and engaging in violent behavior and coping in other dysfunctional ways.
People personally affected by mental illness have become increasingly vocal in communicating both what their life is like with the mental illness and what helps in moving beyond the role of a patient with mental illness.
I think development of communities by speaking for themselves as a strategy for mental health promotion and prevention can restore confidence, hope and the foundation for well-being among the marginalized. That’s how to build resilient communities.
Quoting Lao Tzu becomes imperative here:
Go to the people. Live with them. Learn from them. Love them. Start with what they know. Build with what they have. But with the best leaders, when the work is done, the task accomplished, the people will say ‘We have done this ourselves’.”
At NADA India, that’s how we try to work. Or as the WHO calls it: #Let’s talk.